Obstructive sleep apnea (OSA) affects millions of individuals worldwide, with estimates indicating that around 22 million Americans suffer from this serious condition. Sleep apnea is characterized by repeated interruptions in breathing during sleep, leading to fragmented rest and significant health risks, including cardiovascular problems, daytime fatigue, and impaired cognitive function.
For many patients, traditional sleep apnea treatment such as CPAP therapy has been a standard measure to manage symptoms; however, adherence can be challenging, with about 50% of users discontinuing it within the first year due to discomfort or lifestyle constraints.
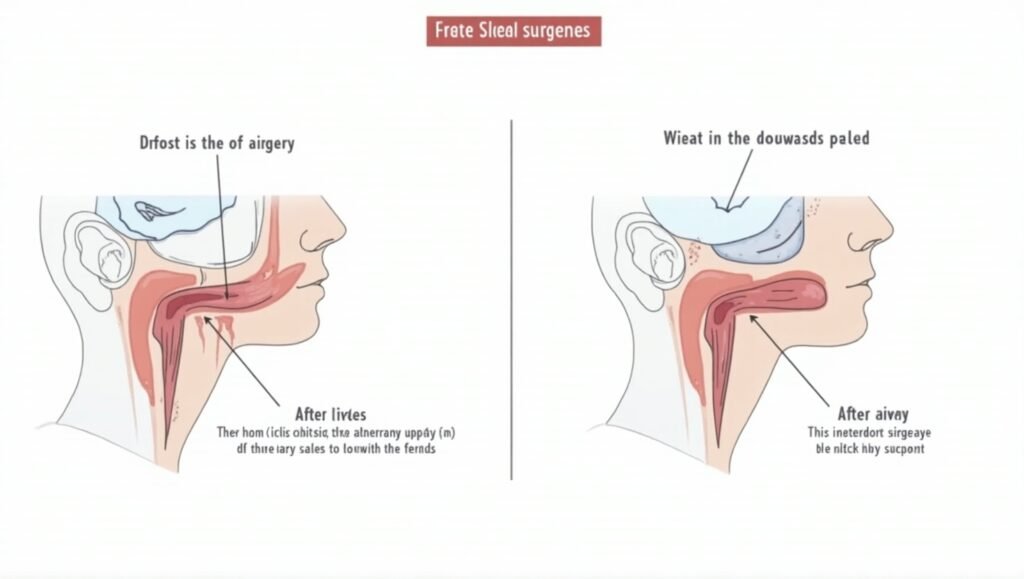
This is where Uvulopalatopharyngoplasty (UPPP) surgery comes into the picture as a potential game changer in surgical options for sleep apnea treatment. UPPP surgery aims to remove excess tissue in the throat, which can block the airway and contribute to sleep apnea symptoms. It not only addresses the physical obstruction but may also eliminate the need for CPAP therapy for many patients.
By facilitating smoother airflow during sleep, UPPP can lead to a noteworthy improvement in sleep quality, enhanced daytime alertness, better mood stability, and increased overall energy levels. For those who have struggled with the challenges of sleep apnea or found traditional treatments inadequate, UPPP surgery represents a promising pathway to reclaim restful nights and improved health. It embodies the benefits of sleep surgery, providing an alternative for those who wish to sleep soundly without the discomfort of devices.
Causes of Obstructive Sleep Apnea
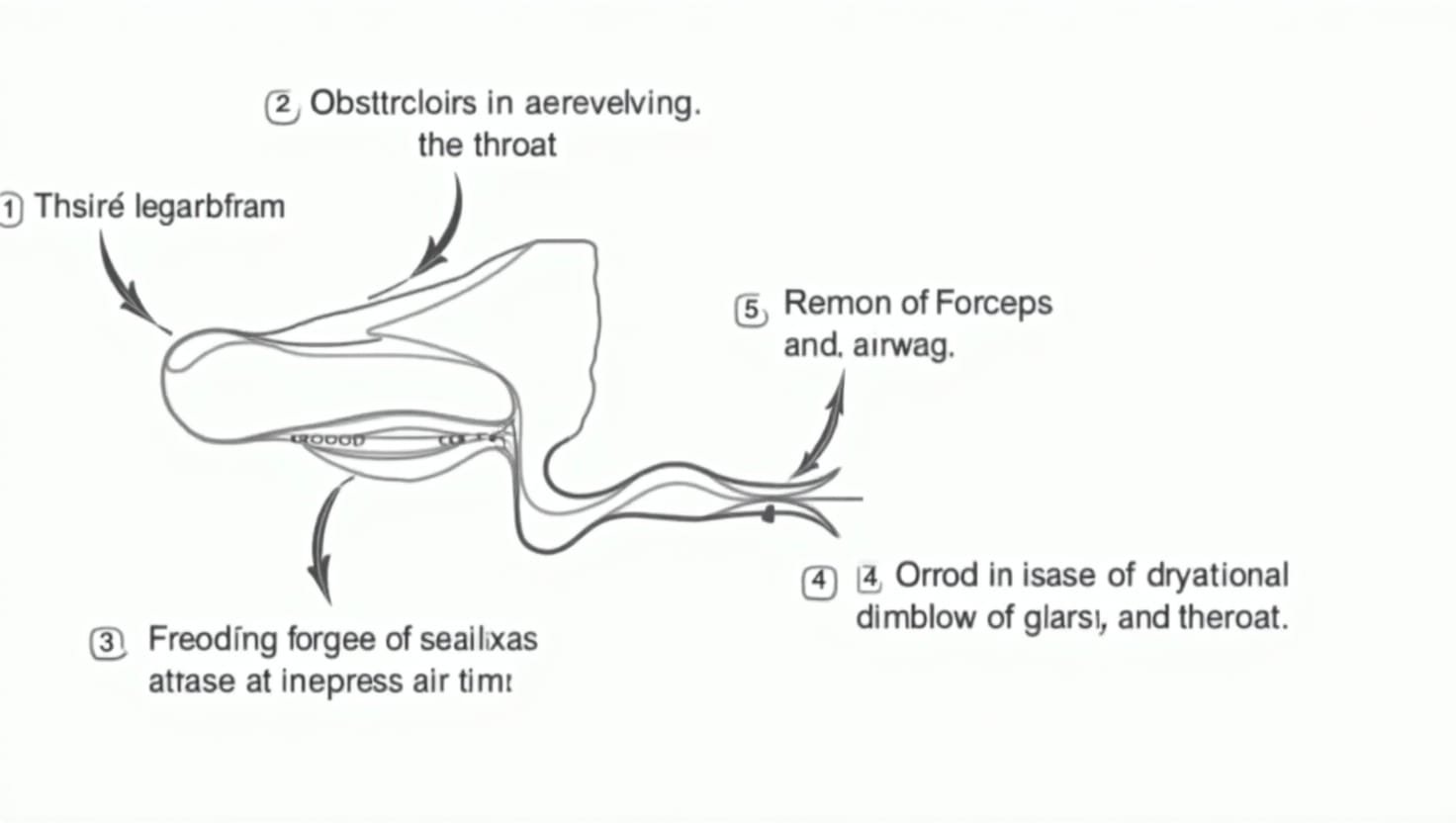
Obstructive sleep apnea (OSA) primarily arises from anatomical and physiological factors that lead to the obstruction of the upper airway during sleep. The condition occurs when the muscles in the throat relax excessively, leading to a narrowing or complete blockage of the airway. Multiple factors can contribute to this relaxation and blockage:
Anatomical Factors
Individuals with a thicker neck circumference, enlarged tonsils, or excess tissue around the throat are at higher risk. In some cases, a deviated septum or an elongated uvula may also contribute to airway obstruction.
- Deviated Septum: A bent or crooked nasal septum can restrict airflow through the nasal passages, making it harder to breathe during sleep. This obstruction can lead to an increased likelihood of snoring and apnea episodes.
- Enlarged Tonsils and Adenoids: Particularly in children, enlarged tonsils and adenoids can block the airway, leading to obstructive sleep apnea.
- Excess Tissue in the Throat: People with a thicker neck circumference or those with excess soft tissue around the throat are also at increased risk. This tissue can collapse during sleep, causing blocked airflow.
Lifestyle Factors
In addition to anatomical issues, certain lifestyle factors also contribute significantly to the development and severity of OSA:
- Obesity: One of the most significant risk factors for OSA is obesity. Excess weight, particularly around the neck, places additional pressure on the airway, increasing the likelihood of obstruction during sleep. Studies indicate that even modest weight loss can significantly improve sleep apnea symptoms.
- Alcohol and Sedatives: These substances can further relax throat muscles, exacerbating airway blockage. Their consumption, particularly before bedtime, can lead to increased incidents of apnea.
- Age and Gender: OSA is more prevalent among older adults, and men are generally more likely to develop this condition than women. Changes in muscle tone and fat distribution with age can increase the risk.
When the airway is obstructed, patients experience repeated episodes of apnea—periods of no breathing that can last from a few seconds to minutes. These interruptions can occur hundreds of times per night, leading to poor oxygen levels, interrupted sleep, and resulting in excessive daytime sleepiness. Moreover, OSA can increase the risk of cardiovascular issues, mood disorders, and cognitive impairments, severely affecting the quality of life.
Urgent and effective intervention is critical for managing obstructive sleep apnea, which is where UPPP surgery comes into play. Uvulopalatopharyngoplasty aims to remove excess tissue in the throat, helping to clear obstructions and allowing for a wider airway. By addressing the root cause of airway blockage, UPPP surgery can significantly improve breathing during sleep and potentially eliminate the need for CPAP therapy, offering a valuable solution for those who have not responded well to conservative treatment options.
Symptoms and Diagnosis of Sleep Apnea
Obstructive sleep apnea (OSA) is often characterized by a range of common symptoms that can significantly impact daily life and overall health. Individuals with OSA frequently experience loud snoring, gasping or choking during sleep, and excessive daytime sleepiness. These symptoms can lead to difficulties with concentration, mood changes, and decreased energy levels, making it challenging to perform daily tasks effectively. Furthermore, the lack of quality sleep can contribute to more severe health issues, such as cardiovascular disease, hypertension, and metabolic disorders.
To diagnose OSA, a thorough medical evaluation is essential. This typically includes a detailed sleep history, a physical examination, and may involve a sleep study (polysomnography), which monitors various body functions during sleep, such as oxygen levels, heart rate, and breathing patterns. Home sleep tests may also be utilized for those who are unable to attend an overnight sleep clinic.
The diagnostic process is crucial, as early detection and intervention can prevent complications associated with untreated OSA. Individuals experiencing symptoms should not hesitate to consult with a healthcare professional. Understanding the severity of their condition and exploring treatment options, including lifestyle changes or, in some cases, surgical interventions like Uvulopalatopharyngoplasty (UPPP), can significantly enhance both sleep quality and overall well-being.
Symptoms and Diagnosis of Sleep Apnea
Obstructive sleep apnea (OSA) is characterized by a variety of common symptoms that can significantly impact daily life and overall health. Individuals with OSA often suffer from loud snoring, episodes of gasping or choking during sleep, and excessive daytime sleepiness. These symptoms can hinder concentration, affect mood stability, and decrease energy levels, which may make completing everyday tasks a struggle. Furthermore, the sleep quality deficits associated with OSA can lead to serious health issues over time, including cardiovascular disease, hypertension, and metabolic disorders.
Diagnosing OSA requires a comprehensive medical evaluation. This typically involves a detailed sleep history, physical examination, and often a sleep study, known as polysomnography. This study monitors several physiological functions during sleep, including oxygen levels, heart rate, and breathing patterns. In some cases, home sleep tests may be utilized for individuals who cannot attend an overnight sleep clinic.
The diagnostic process is vital because early detection and intervention can prevent serious complications associated with untreated OSA. Individuals experiencing symptoms should promptly consult with healthcare professionals to understand the severity of their condition and explore treatment options. These may include lifestyle changes or surgical interventions like Uvulopalatopharyngoplasty (UPPP). Effectively diagnosing and treating OSA can lead to significant improvements in both sleep quality and overall well-being, reassuring patients on their journey to better health.
Key Symptoms of Obstructive Sleep Apnea
- Loud Snoring: Often a noticeable indicator, affecting sleep quality for both the individual and their partner.
- Gasping or Choking: Episodes may occur during sleep when airflow becomes obstructed, waking the individual briefly.
- Excessive Daytime Sleepiness: Persistent tiredness and fatigue, leading to difficulties with concentration and mood stability during the day.
- Difficulty Concentrating: Cognitive impairment due to disrupted sleep can affect performance in daily tasks.
- Mood Changes: Increased irritability and mood swings may arise from the effects of poor sleep quality.
- Reduced Energy Levels: Overall feelings of lethargy due to interrupted sleep patterns.
These symptoms can diminish quality of life and may contribute to severe health risks if left untreated, highlighting the importance of diagnosis and intervention.
Benefits of UPPP Surgery
Uvulopalatopharyngoplasty (UPPP) surgery offers numerous advantages for individuals suffering from obstructive sleep apnea (OSA) and chronic snoring. Here are some of the key benefits:
- Improved Sleep Quality: By removing tissue that obstructs the airway, UPPP helps to facilitate uninterrupted breathing during sleep, resulting in deeper and more restorative sleep cycles. Many patients report a significant increase in their overall sleep quality following surgery.
- Reduction in Snoring: One of the most immediate benefits of UPPP is the notable decrease in snoring. This can not only improve the quality of life for the individual but can also create a quieter sleeping environment for partners and family members.
- Increased Daytime Alertness: With better sleep quality comes increased daytime alertness. Many individuals who undergo UPPP report feeling more awake and alert during the day, which can enhance productivity and safety, especially in high-stakes environments like driving or operating machinery.
- Potential Improvements in Mood and Energy Levels: Improved sleep can lead to better emotional regulation, reducing instances of mood swings, irritability, and anxiety. Patients often experience a boost in energy levels making daily activities more manageable and enjoyable.
- Reduced Dependence on CPAP Therapy: For patients who have struggled with CPAP (Continuous Positive Airway Pressure) therapy, UPPP can provide an alternative solution. In many cases, UPPP surgery may eliminate or significantly reduce the need for CPAP machines, freeing individuals from constraints and discomfort associated with nightly wear.
These benefits underscore the value of considering UPPP surgery for individuals who consistently battle obstructive sleep apnea and its associated challenges. With a range of positive impacts on sleep, alertness, and overall health, UPPP surgery could be a turning point for many patients seeking relief from the burdens of this condition.
| Aspect | UPPP Surgery | CPAP Therapy |
|---|---|---|
| Effectiveness | Can eliminate or reduce symptoms of OSA | Effective in managing OSA but may not eliminate it |
| Patient Comfort | May involve post-operative discomfort but lasts | Can be uncomfortable and requires wearing a mask or device during sleep |
| Lifestyle Impact | Allows for a return to normalcy without nightly devices | Requires ongoing nightly use, impacting sleep routines and travel |
| Long-term Solution | Can provide a permanent solution for some patients | May require long-term adherence and ongoing adjustments |
| Snoring Reduction | Significantly reduces or eliminates snoring | May not reduce snoring for all users |
| Aspect | UPPP Surgery | CPAP Therapy |
|---|---|---|
| Effectiveness | Can eliminate or reduce symptoms of OSA | Effective in managing OSA but may not eliminate it |
| Patient Comfort | May involve post-operative discomfort but lasts | Can be uncomfortable and requires wearing a mask or device during sleep |
| Lifestyle Impact | Allows for a return to normalcy without nightly devices | Requires ongoing nightly use, impacting sleep routines and travel |
| Long-term Solution | Can provide a permanent solution for some patients | May require long-term adherence and ongoing adjustments |
| Snoring Reduction | Significantly reduces or eliminates snoring | May not reduce snoring for all users |
Patient Testimonials
Success Stories
- Sarah T., a 42-year-old teacher, shared her experience: “After struggling with severe sleep apnea for years and being unable to tolerate CPAP, I chose UPPP surgery. I can’t express how much it has changed my life! My snoring has dramatically decreased, and I sleep through the night without interruptions. I wake up feeling refreshed and ready for the day!”
- Mark L., a 50-year-old engineer, recounted: “I was skeptical about surgery, but I was desperate for relief. The UPPP procedure was straightforward, and the recovery was manageable. It’s been six months since my surgery, and I have noticed a significant improvement in my overall energy levels. I can finally keep up with my kids!”
- Linda K., age 36, said: “Choosing UPPP was one of the best decisions I’ve made. I no longer suffer from terrible snoring and finally enjoy a deep sleep. I feel happier and more productive at work. It’s incredible what a good night’s sleep can do to transform your life!”
Cautionary Tales
While many patients report positive outcomes, there are some who have faced continued challenges:
- James R., a 47-year-old patient, mentioned: “I hoped UPPP would be my final solution after years of struggling with CPAP. While I did get some relief, I’ve noticed some return of my apnea symptoms and still need to use CPAP occasionally. It’s frustrating to work so hard and not have it fully resolve.”
- Nancy P., age 62, highlighted: “The surgery helped reduce my snoring a lot, but I still have difficulty swallowing. There are days when I feel like I need CPAP again. I wish I had better foresight regarding the potential side effects.”
These testimonials demonstrate that while UPPP surgery has transformed lives for many, it’s essential to approach it with realistic expectations. Individual outcomes can vary based on several factors, including anatomy and adherence to post-operative care.
For anyone considering UPPP, it is important to consult with a qualified medical professional to ensure it is the right solution for their specific needs.
Patient Testimonials
Success Stories
- Sarah T., a 42-year-old teacher, shared her experience: “After struggling with severe sleep apnea for years and being unable to tolerate CPAP, I chose UPPP surgery. I can’t express how much it has changed my life! My snoring has dramatically decreased, and I sleep through the night without interruptions. I wake up feeling refreshed and ready for the day!”
- Mark L., a 50-year-old engineer, recounted: “I was skeptical about surgery, but I was desperate for relief. The UPPP procedure was straightforward, and the recovery was manageable. It’s been six months since my surgery, and I have noticed a significant improvement in my overall energy levels. I can finally keep up with my kids!”
- Linda K., age 36, said: “Choosing UPPP was one of the best decisions I’ve made. I no longer suffer from terrible snoring and finally enjoy a deep sleep. I feel happier and more productive at work. It’s incredible what a good night’s sleep can do to transform your life!”
Cautionary Tales
While many patients report positive outcomes, there are some who have faced continued challenges:
- James R., a 47-year-old patient, mentioned: “I hoped UPPP would be my final solution after years of struggling with CPAP. While I did get some relief, I’ve noticed some return of my apnea symptoms and still need to use CPAP occasionally. It’s frustrating to work so hard and not have it fully resolve.”
- Nancy P., age 62, highlighted: “The surgery helped reduce my snoring a lot, but I still have difficulty swallowing. There are days when I feel like I need CPAP again. I wish I had better foresight regarding the potential side effects.”
These testimonials demonstrate that while UPPP surgery has transformed lives for many, it’s essential to approach it with realistic expectations. Individual outcomes can vary based on several factors, including anatomy and adherence to post-operative care.
For anyone considering UPPP, it is important to consult with a qualified medical professional to ensure it is the right solution for their specific needs.
In conclusion, Uvulopalatopharyngoplasty (UPPP) surgery presents a valuable opportunity for individuals grappling with obstructive sleep apnea (OSA) and the associated challenges of chronic snoring. By effectively addressing the anatomical obstructions in the throat, UPPP not only enhances sleep quality but significantly reduces or eliminates snoring, allowing for more restful nights. Many patients experience a notable improvement in daytime alertness, mood stability, and energy levels following the procedure.
Moreover, for individuals who have struggled with CPAP therapy or found it unsuitable, UPPP offers a promising alternative. The potential to reduce or eliminate reliance on CPAP means reclaiming a more comfortable, unrestricted night’s sleep. While each person’s experience may vary, the numerous success stories underline the procedure’s positive impact on health and quality of life.
If you are considering UPPP surgery, it is essential to consult a qualified healthcare professional who can conduct a thorough evaluation and help determine if this procedure is the right fit for your unique needs. You deserve the path towards better sleep and improved overall well-being, so don’t hesitate to seek the guidance and support you need.
For a deeper understanding of treatments available for obstructive sleep apnea (OSA), including detailed discussions on Uvulopalatopharyngoplasty (UPPP) and other methods, visit reputable sources like the Mayo Clinic’s overview of OSA treatments and insights from the American Association of Oral and Maxillofacial Surgeons. These resources provide comprehensive details on surgical and non-surgical treatment approaches that may complement the information discussed in this article.